Kathy Martino, former FFL Board Member
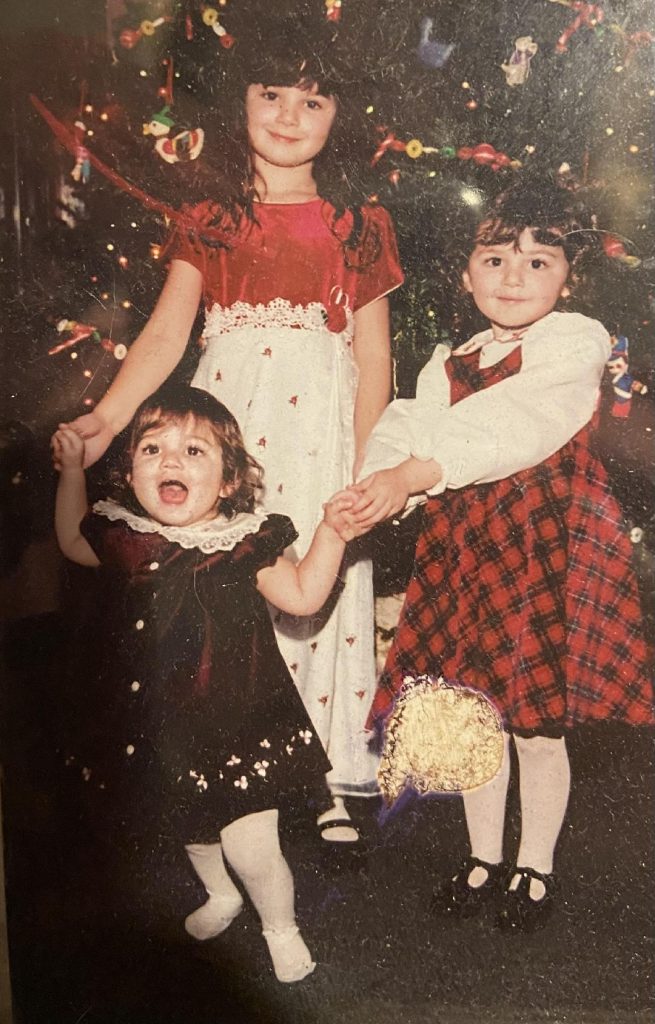
Twenty years ago, while I was busy raising my 4-year-old daughter, Kailyn and my 1-year-old daughter, Sarah, I joyfully discovered I was pregnant with my third child. My husband, Michael, and I, were thrilled to be expanding our family and were eager to add to the loving chaos of our home.
At my first ultrasound, I discovered that this pregnancy and delivery would be complicated and scary. My placenta was low-lying in my uterus, completely covering the cervix, which is the baby’s exit door. This rare complication, called placenta previa, can cause serious complications, including hemorrhaging during pregnancy which can prompt bedrest, hospitalization, and sometimes emergency preterm delivery. With a full previa, which I had, a c-section was mandatory. Typically, women need to avoid exercise, heavy lifting, and exhausting themselves, and even when they do, heavy preterm bleeding is still common and requires immediate medical attention.
My first thoughts were “How do I avoid tiring myself out while chasing after a preschooler and a toddler? Sarah is young enough to need to be lifted and carried around every day. How would I care for my girls if I need to go on bedrest? What if I start to hemorrhage at home and need emergency help?” It was reassuring to know that I had a loving husband and local parents for support, but I still worried. As the months went by, and my pregnancy was progressing, I was trying to not overexert myself, but when my girls needed me, I was there for them. Every time I picked up Sarah, I would wonder if this might prompt bleeding and a rushed visit to the hospital.
Throughout the pregnancy, I was being monitored by two wonderful pro-life women OBGYNs, one of whom was the consulting OBGYN for our local pregnancy resource center. My husband, who is an emergency physician, was familiar with the risks and complications common to placenta previa. He questioned our OBGYNs repeatedly about what problems we should prepare for, including planning for an early c-section delivery, as common medical practice was to deliver early with full placenta previa. Our doctors were surprisingly relaxed. They told us, “We’re aware of the usual statistics, including how commonly the severe bleeding occurs, but that is not our experience with our patients.” When Michael and I looked confused, they added “We pray for our patients. Of course, we’ll watch over you closely, and we’re prepared to intervene if needed, but our practice just hasn’t seen the problems typical with previa.”
Remarkably, I had no previa symptoms at all throughout the pregnancy, despite the physical demands of raising my young girls. At the full 40 weeks, my two OBGYNs shared the c-section surgery to deliver our third daughter, Isabella Grace. I’m so proud to share that she is now an engaged college student interning at Feminists for Life. I remain forever grateful to my two amazing OBGYNs – strong prolife women who were examples to me of genuine caring, professional excellence, and abiding faith.